Frequently Asked Dietary Questions in IBD
Key points
- Food has not yet been proven to cause IBD.
- A healthy balanced diet is the best way to eat for IBD.
- There are no specific foods that everyone with IBD needs to avoid.

This dietary resource developed by GI DREAM provides general dietary information for people with Inflammatory Bowel Disease (IBD).
1. Has food caused my IBD?
The cause of IBD remains unknown. Food has not yet been proven to cause IBD. A significant amount of research is occurring in this area.
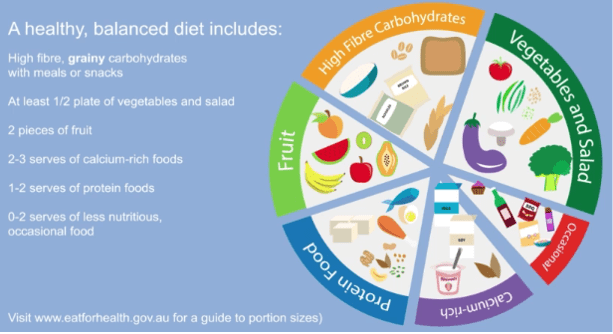
2. Should I follow a particular diet to help my IBD?
A healthy balanced diet is the best way to eat for IBD. The GESA Diet and IBD consumer Information sheet and GI Dream Eating Well with Crohn’s disease and ulcerative colitis videos provide useful dietary information on eating well with IBD.
An IBD dietitian can help you tailor this general dietary advice to your personal needs.
3. Are there any particular foods I need to avoid for my IBD?
In general, there are no specific foods that everyone with IBD needs to avoid. Some studies suggest that limiting red and processed meats may help reduce the risk of flares in ulcerative colitis. For Ulcerative Colitis and Crohn’s disease, limiting highly processed foods in line with healthy eating guidance may be beneficial. Some people find it harder to digest certain foods. If you think certain foods or beverages may be causing gut symptoms, an IBD dietitian can identify potential trigger foods, what you can eat and how much of a trigger food you can eat before a symptom occurs. This type of individualised, expert IBD dietary guidance ensures you continue to consume the right amount of nutrition and keeps eating enjoyable without unnecessary food avoidance.
4. Should I avoid gluten or dairy for my IBD?
There is no evidence that gluten or dairy cause or worsen inflammation in IBD. However, In some people, the fibre in wheat (fructans) or the natural sugar in milk (lactose) may trigger gut symptoms without causing inflammation. This does not mean you need to avoid these foods completely. If you think wheat, gluten or dairy make your gut symptoms worse, talk to an IBD dietitian.
5. Do I need to avoid fibre for my IBD?
For most people with IBD, fibre is safe and beneficial. Eating a wide range of fibrous foods from fruits, vegetables, wholegrains, legumes, nuts and seeds every day is good for your physical, gut and mental health. Different fibres can absorb water, form gels, add bulk to stools or ferment in the large bowel. Fibre helps the bowel work well and specific fibres may reduce symptoms of diarrhoea and constipation. The exception to this general fibre rule is if you have symptoms such as bloating and constipation that is due to narrowing of the bowel (strictures). An IBD dietitian can personalise this fibre advice for your bowel function and symptoms.
6. Are there any foods I can eat to help keep my disease in remission?
In general, a well-balanced, varied diet in addition to prescribed IBD medications is an important first dietary step for managing inflammation. Fibre may have a protective role in keeping inflammation under control in IBD. An IBD dietitian can explain which types of fibres might help to control inflammation as this is different for Crohn’s disease and ulcerative colitis.
7. What should I eat during a flare of my disease?
During a flare, inflammation is the main driver of gut symptoms (abdominal pain, change in bowel habits and bleeding). Inflammation can affect the digestion of food. While certain foods may be harder to tolerate during flares, the key is to treat the inflammation itself so that digestion improves. The most important first step is to speak to your gastroenterologist or IBD nurse about which therapy is best to treat inflammation. For some people with a flare of Crohn’s disease, Exclusive enteral nutrition can treat the inflammation in place of, or in conjunction with, medical therapy. There is not yet a specific diet to treat ulcerative colitis during a flare.
Some general tips for eating well during a flare:
- Listen to your body, choose foods that feel easier to digest
- Continue eating a well-balanced, varied diet as best you can
- Avoid the temptation to cut out groups of foods to see if they help
- Talk to an IBD dietitian for individualised dietary strategies
- Monitor your weight, and speak with your IBD team if you are losing weight
8. Are there certain foods that will reduce how often I have diarrhoea and am running to the toilet?
There are different dietary strategies that may help these symptoms. Choosing the right dietary strategy depends whether diarrhoea and urgency are caused by inflammation or other causes if your inflammation is in remission (e.g. irritable bowel). An IBD dietitian can help you to identify food triggers or eating patterns that are contributing to troublesome symptoms whilst also ensuring your diet remains nutritionally balanced.
9. I feel tired all the time, what can I eat to help with this?
Fatigue is a common symptom of IBD. Firstly, it is important to make sure you do not have anaemia. Your doctor can check this through a blood test. Fatigue can also be caused by poor sleep, changes in mental health, some medications, not eating well, or losing weight and muscle strength. Speak with your doctor or IBD dietitian about your fatigue so an appropriate plan can be developed.
10. My appetite is poor and I do not feel like eating. What should I do?
Trying to eat small, nutritious meals or snacks every 2-3 hours. If your appetite remains poor, you are losing weight or have low energy levels, it is important to talk to an IBD dietitian for individualised strategies.
11. Why am I losing weight and what can I do about it?
Inflammation can cause weight loss by increasing your energy needs, reducing appetite, and affecting energy and protein absorption. If food is being avoided to try and manage symptoms, it may lead to weight loss and reduced muscle strength. Speak to your IBD dietitian who can help with strategies to prevent and regain weight and muscle loss.
12. Are there natural remedies that can heal my gut?
Caution should be taken here as many promoted “gut-healing” remedies or supplements have not been scientifically studied. Some supplements can interfere with medications or cause other health complications. Speak to your doctor, pharmacist or IBD dietitian before trying any natural therapies to ensure you are being safe and not spending money on items that may not have a beneficial effect.

Acknowledgements:
This resource was developed in 2022 by the DECCAN Education Materials Working Group and reviewed by the GI DREAM Board in line with ECCO Consensus on Dietary Management of IBD (2025). Requests and enquiries about this document should be directed to [email protected] or website www.gidream.org. GI DREAM does not take any liability for any injury, loss or damage incurred by the use or reliance on this information. Reviewed August 2025. Date for review August 2027.