Frequently Asked Dietary Questions in IBD
Key points
- Food has not yet been proven to cause IBD.
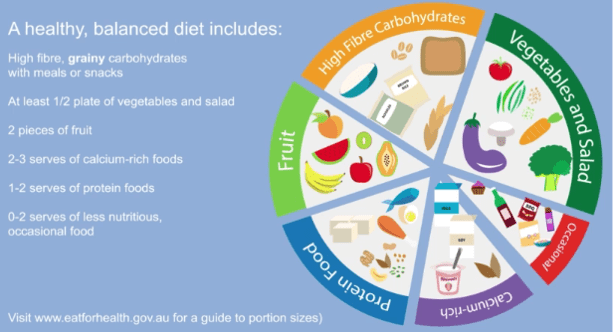
- A healthy balanced diet is the best way to eat for IBD.
- There are no specific foods that everyone with IBD needs to avoid.

This dietary resource developed by DECCAN provides general dietary information for people with Inflammatory Bowel Disease (IBD).
1. Has food caused my IBD?
The cause of IBD remains unknown. Food has not yet been proven to cause IBD. A significant amount of research is occurring in this area.
2. Should I follow a particular diet to help my IBD?
A healthy balanced diet is the best way to eat for IBD. The GESA Diet and IBD consumer Information sheet and DECCAN Eating Well with Crohn’s disease and ulcerative colitis videos provide useful dietary information on eating well with IBD.
An IBD dietitian can help you tailor this general dietary advice to your personal needs.
3. Are there any particular foods I need to avoid for my IBD?
In general, there are no specific foods that everyone with IBD needs to avoid. There is some research suggesting limiting red and processed meats may help to control inflammation in ulcerative colitis. Some people do, however, find it harder to digest certain foods. If you think certain foods or beverages may be causing gut symptoms, an IBD dietitian can identify potential trigger foods, what you can eat and how much of a trigger food you can eat before a symptom occurs. This type of individualised, expert IBD dietary guidance ensures you continue to consume the right amount of nutrition and keeps eating enjoyable without unnecessary food avoidance.
4. Should I avoid gluten or dairy for my IBD?
There is no scientific evidence that gluten or dairy cause inflammation or make inflammation harder to control in IBD. In some people, the fibre in wheat (fructans) and the natural sugar in milk (lactose) can cause gut symptoms, but not inflammation. This does not mean you need to avoid these foods completely. If you think wheat, gluten or dairy make your gut symptoms worse, talk to an IBD dietitian.
5. Do I need to avoid fibre for my IBD?
Fibre does not usually need to be avoided in IBD. A eating a wide range of fibrous foods from fruits, vegetables, wholegrains, legumes, nuts and seeds every day is good for your physical and mental health. Different fibres can absorb water, form gels, add bulk to stools or ferment in the large bowel. Fibre helps the bowel work well and specific fibres may reduce symptoms of diarrhoea and constipation. The exception to this general fibre rule is if you have symptoms such as bloating and constipation that is due to narrowing of the bowel (strictures). An IBD dietitian can personalise this fibre advice for your bowel function and symptoms.
6. Are there any foods I can eat to help keep my disease in remission?
In general, a well-balanced, varied diet in addition to IBD medications is an important first dietary step for managing inflammation. Fibre may have a protective role in keeping inflammation under control in Crohn’s disease and ulcerative colitis. An IBD dietitian can explain which types of fibres might help to control inflammation as this is different for Crohn’s disease and ulcerative colitis (UC).
7. What should I eat during a flare of my disease?
During a flare, inflammation causes gut symptoms (abdominal pain, change in bowel habits and bleeding), not foods. Inflammation can affect the digestion of food. If inflammation is treated, symptoms of poor digestion will improve. The most important first step is to speak to your IBD nurse or doctor about which therapy is best to treat this inflammation. For some people with Crohn’s disease Exclusive enteral nutrition can treat the inflammation in place of or in conjunction with medical therapy. However we don’t yet have a specific diet to treat UC during a flare.
Some general tips for eating well during a flare:
- Listen to your body, choose foods that feel easier to digest
- Continue eating a well-balanced, varied diet as best you can
- Avoid the temptation to cut out groups of foods to see if they help
- Talk to an IBD dietitian for individualised dietary strategies
- Monitor your weight, if you are losing weight speak with your IBD team
8. Are there certain foods that will reduce how often I have diarrhoea and am running to the toilet?
There are different dietary strategies that may help these symptoms. Choosing the right dietary strategy depends whether diarrhoea and urgency are being caused by inflammation or other causes (e.g. irritable bowel) if your inflammation is in remission. An IBD dietitian can help you to identify food triggers or eating patterns that are contributing to troublesome symptoms whilst also ensuring your diet remains nutritionally balanced.
9. I feel tired all the time, what can I eat to help with this?
Fatigue is a common symptom of IBD. Firstly, it is important to make sure you do not have anaemia. Your doctor can check this through a blood test. Fatigue can also be caused by poor sleep, changes in mental health, not eating well, or losing weight and muscle strength. Speak with your doctor or IBD dietitian about your fatigue so an appropriate plan can be developed.
10. My appetite is poor and I do not feel like eating. What should I do?
Trying to eat small, nutritious meals or snacks every 2-3 hours. If your appetite remains poor, you are losing weight or have low energy levels, it is important to talk to an IBD dietitian for individualised strategies.
11. Why am I losing weight and what can I do about it?
Inflammation can cause weight loss as it can affect how much energy and protein eaten and absorbed, due to poor appetite and increased nutritional needs. If food is being avoided to try and manage symptoms it may lead to weight loss and reduced muscle strength. Speak to your IBD dietitian who can help with strategies to prevent and regain weight and muscle loss.
12. Are there natural remedies that can heal my gut?
Caution should be taken here as many promoted gut-healing remedies or supplements have not been scientifically studied. Some remedies can interfere with medications or cause other health complications. Speak to your doctor, pharmacist or IBD dietitian before trying any natural therapies to ensure you are being safe and not spending money on items that may not have a beneficial effect.

Acknowledgements:
This resource was developed in 2022 by the DECCAN Education materials working group that included the following Accredited Practicing Dietitians: Alice Day, Jessica Fitzpatrick, Emma Halmos, Katherine Healy, Liz Purcell, Emily Hunt, Rumbidzai Mutsekwa, Nadia Shadid, Clara Newsome, Sarah Phillips, Emma Landorf. Requests and enquires about this document should be directed to [email protected] or website www.deccanibd.org. DECCAN does not take any liability for any injury, loss or damage incurred by the use or reliance on this information.
Developed January 2023. Date for review December 2024.
