Have you used our translated resources? We want to hear from you
We currently have funding from the Australian Government to increase our offering of IBD resources in other languages.
We want to hear from our community about the type of translated resources you’d like to see on the CCA website. For instance, more webpages, videos, or languages not currently offered.
Please contact [email protected] if you are interested in helping us expand our multilingual resources.
Inflammatory Bowel Disease (IBD) is an inflammatory condition that affects the bowel, and its cause is complex and not well understood. It is thought that factors such as genetics, environmental influences, and the gut microbiome affect the risk of developing IBD. Some environmental factors that can contribute to the development of IBD include the presence of heavy metals, pesticides, organic pollutants, and air pollution. Heavy metals such as copper, lead, and cadmium can alter the gut microbiome and lead to a ‘leaky gut’ (the damaged lining of the small intestine allows bacteria and foreign substances to enter the bloodstream). Patients with IBD generally have higher concentrations of these metals than people in the general population. Pesticides and organic pollutants can also affect the gut microbiome and contribute to a ‘leaky gut.’
Long-term exposure to air pollution has been linked to the development of not only respiratory conditions but also other inflammatory disorders such as rheumatoid arthritis and multiple sclerosis, which have similar disease development processes to IBD. These factors are thought to have contributed to a 47.5% increase in global IBD cases, from 3.3 million in 1990 to 4.9 million in 2019.
A 2024 literature review of current research regarding the development of IBD and air pollution found correlations with multiple types of gases produced by air pollution. The gases in air pollution include carbon dioxide, nitric oxides, and particulate matter (PM) of varying sizes, which can be produced by cars, factories, and forest fires. For reference, air pollution levels in Australia are generally low, with cities such as Melbourne having an average PM 2.5 of 6.5 μg/m³, below the Australian government target of 8 μg/m³. However, this can increase dramatically, such as during the 2019-2020 bushfires, peaking at 470 μg/m³ on January 14, 2020.
PM particles, once breathed into the lungs, are cleared into the intestine, where they can produce inflammatory molecules and interact with the gut microbiome. Specifically, exposure to PM 2.5 has been associated with IBD, and with increases in PM 2.5 exposure, the chance of needing intestinal surgery increases. Countries with higher air pollution overall have a higher rate of hospitalizations for IBD patients, with every increase of ten units associated with a 40% increase in hospitalizations. Nitric dioxide pollution was also associated with an increase in overall mortality in IBD patients.
More research is needed to investigate the exact disease processes that each air pollutant contributes to the development of IBD, as well as the duration, amount, and length of exposure to air pollution needed to cause them.
Any information provided in this article is not intended as medical advice. If you have any concerns or questions, we recommend discussing them with your doctor.
Global Perianal Crohn’s Disease – research survey
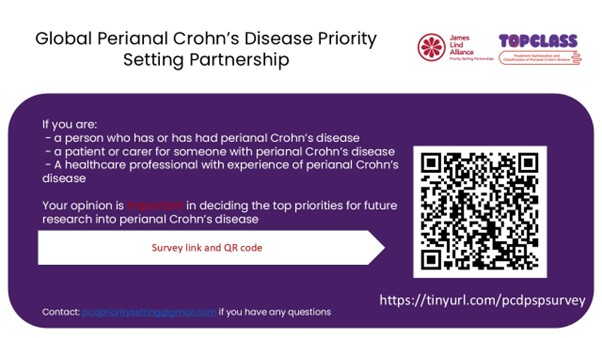
Researchers are seeking to identify the top priorities for people living with perianal Crohn’s Disease. We are inviting people to participate in a brief survey to highlight the most crucial areas for future research. This will guide future studies, ensuring they address the most key issues raised by those with lived or professional experience of perianal Crohn’s disease.
If you have personal experience with perianal Crohn’s, are a parent or caregiver for someone with the condition, or are a healthcare professional with relevant experience, please complete this short survey.
https://imperial.eu.qualtrics.com/jfe/form/SV_3VJwYuL6VK2jc90

The Age and The Sydney Morning Herald recently published a piece about love and dating with Inflammatory Bowel Disease.
In the lead up, we placed a call out on social media for potential interview subjects. The response was overwhelming, demonstrating the interest in this particular topic. We thank everyone who got in touch to express their interest!
You can read the article here.
Image: Natasha Jiwani with dog Rummy. Image Credit: Nine Entertainment Co/ James Brickwood

We’re thrilled to have been nominated as a finalist for the Research Australia Health & Medical Research advocacy awards 2024!
It’s fantastic recognition of the work we do, and it reflects the incredible and consistent advocacy from the IBD community.
You can see the full nomination list here.
Source: efcca.org/sites/default/files/HUCUK brosura 2021 EN LowRes_0.pdf (pg 60)
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
Ingredients (serves 2):
• 1/2 cup of quinoa (85 g)
• One tablespoon of olive oil
• One medium-sized courgette
• a handful of baby spinach
• 200 g of chicken fillet
• Salt
• A bit of chicken stock
• Herbs of choice
Preparation:
Rinse the quinoa, put it in the pot and pour a full cup of water over it.
While the quinoa is cooking, fry the courgettes chopped into rounds on 1 tablespoon of olive oil. After 5 minutes, add the diced chicken, that you have
salted beforehand, into the pan. Add a bit of chicken stock or water and let it simmer over medium heat. Finally, add spinach into the pan, and let it wilt. Add more salt, if needed. When the quinoa is cooked, add 1 tablespoon of olive oil. When the courgettes and chicken are ready (20 – 30 minutes), add cooked
quinoa to the pan and add your spices of choice. This can be served both hot and cold
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
Poached salmon with carrot and celery purée (source: EFCCA)
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
Poached salmon
Ingredients (serves 2):
Skinless salmon fillet, 2 pieces
• white wine, 100 mL
• 1 large shallot, chopped into large pieces
• 1 bay leaf
• salt
Carrot and celery purée
Ingredients (serves 2):
• celery root, 200 g
• carrots, 200 g
• butter or olive oil, 10 – 15 g
• 1/4 teaspoon of salt
Preparation for the salmon
Put salmon fillets in a sauté pan. Add the shallot, bay leaf, wine, and boiling water to the pan, so that it covers the salmon fillets.
Simmer over low heat for about 10 minutes. Remove the salmon from the pan, put it on a serving plate, dry it with a paper towel and add a pinch of salt. In the
meantime, prepare the carrot and celery purée and sweet potato chips. Poached salmon with carrot and celery purée and sweet potato chips should be served
with a watercress salad with lemon juice dressing, and a drizzle of olive oil.
Preparation for the puree
Boil the celery root and carrots in a bit of water, drain the boiled vegetables, add a bit of butter or oil, add some salt and mash them into a purée.
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
Image source: Unsplash
PBS listing of Velsipity for treatment of UC
Pfizer Australia has announced the reimbursement of its oral S1P receptor modulator on the PBS for the treatment of moderate to severe active Ulcerative Colitis, as reported by Pharmacy Daily.
The PBS has listed Velsipity (etrasimod), which is indicated for adults with an inadequate response, loss of response or intolerance to conventional, biologic or JAK inhibitor therapies.
CCA CEO Leanne Raven welcomed the PBS listing.
“It’s encouraging to see treatments like Velsipity listed on the PBS, providing another subsidised treatment option for those who need it,” Raven said.
Expanded access to funded shingles vaccine
The federal government has expanded access to the shingles vaccine to cover individuals aged 18 to 64 who are at a moderate to high risk of herpes zoster as advised by the ATAGI.
Leanne Raven, Chief Executive Office, Crohn’s and Colitis Australia said that Australians living with auto-immune diseases such as Crohn’s or Ulcerative colitis need as much support as possible to avoid developing conditions that can further impact their day-to-day life.
“This is especially important for those who have to take certain immunosuppressants, as they are at an even greater risk of developing other health conditions such as infections, or cardiovascular disease depending on their treatment.”
Patients are encouraged to talk to their GP or gastroentorologist about their eligibility for this vaccine.
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
Ingredients (serves 2):
• 2 large slices of homemade sourdough bread
• extra virgin olive oil
• 12 asparagus (green, cultivated or wild asparagus)
• 2 large free-range eggs
• Parmesan cheese (optional)
Preparation:
Toast the bread in the pan, over high heat. Once it is crisp and golden brown, remove it from the pan to a plate or board, and brush it with some olive oil. Remove the woody ends of the asparagus and blanch them in salted water for up to 5 minutes. Drain the asparagus and put them on top of the toasted bread.
Poach two eggs for a couple of minutes in water with some salt and vinegar. Put each egg over the
asparagus, and sprinkle with a bit of parmesan cheese (optional)
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
“I know now that I am stronger” – Trish’s story
Trish shared her story a few months after completing the Gold Coast Marathon in July 2024.

I was diagnosed when I was 15.
It feels like it happened over night. One minute I was fine, then I was going to the toilet 10-plus times a day. I would eat and immediately have to go to the toilet. Due to my age and the rapid weight loss I was experiencing, my parents thought i had an eating disorder. They couldn’t believe I needed to go to the bathroom so quickly after eating.
I grew up in Ireland and it took me over six months to get an appointment with a specialist. I am very fortunate that my parents had private health insurance. It took a bit of time, but I was eventually diagnosed with ulcerative colitis. This diagnosis changed to Crohn’s Disease. I am fortunate that my dad has colitis. He was a huge help when it came to understanding what was going on.
Following the diagnosis, I had access to a gastroenterologist and that was about it. Looking back, I should have been offered support from a psychologist and a dietitian. So many times, I was told that my symptoms weren’t related to food, which I do not believe to be true. About 25 years on from my diagnosis, there is so much more education and assistance available to people. Here in Australia, I think we are taking care of well and are provided with lots of treatment options.
Now aged 40, I feel I am the healthiest I’ve ever been and am more in control of the disease. I follow a healthy diet, and have an active lifestyle, which has made a massive improvement to my health and wellbeing. I’ve reduced my alcohol intake and do most of my own cooking.
Running has become a new outlet for me.
Exercise has been a big part of my life since Covid-19.
During lockdowns, I decided to make the most of the extra time I had. This started with a yoga challenge and slowly progressed to working out. Each week I felt my energy improve, and I felt I was in a better head space, which reduced my stress as well. I don’t think I realised that –with all these little changes to my lifestyle — I was feeling less bloated, i was going to the bathroom with healthier regularity. My sleep was so much better too.
I started running about three years ago. I couldn’t run 10 minutes without stopping but, with the help and motivation from my husband, I signed up for my first half marathon.
Over the last three years I have completed two half marathons and one full marathon and have booked my next half marathon in November. I run three to four times a week, with some of my runs lasting over three hours. I’ve found this to be great for my mind, but it definitely can take its toll on the body. I have learned that listening to my body is a priority. I need to rest when I am tired and fuel my body with good food. I am fortunate that another passion of mine is cooking so I cook all my food fresh and find alternative recipes to make sure the food I cook healthy and delicious.
The main thing I’ve learned in running marathons is that I’m more than my disease.
Sometimes you can let it take over your life and at times life can feel quite dark. I’ve spent time hooked up to a drip to take Infliximab and feeling sorry for myself. I’ve also been airlifted to hospital because I’ve suspected a bowel perforation.
I know now that I am stronger. I will have bad days as well as great days — and the good days generally outweigh the bad. Keeping myself healthy for myself and my family is number one. I have also learned that letting others help me and support me is not a sign weakness.
We are very fortunate to have so much information and medication options available to us. Listen to your body and trust your instincts. as you will know what works best for you.
Everyone has different symptoms and different triggers so find out what works for you.
