Survey: Sexual and reproductive health needs of women who live in Australia with Inflammatory Bowel Disease.
Researchers at Western Sydney University and Auckland University of Technology want to understand what the sexual and reproductive health needs are of women who live in Australia with the chronic condition of Inflammatory Bowel Disease.
If you have a diagnosis of Inflammatory Bowel Disease, and would like to have your voice heard, please contact the research team at Western Sydney University using the email address: [email protected]
Any information you provide will be treated confidentially and will be used to inform strategies that enhance awareness about the sexual and reproductive health issues associated with inflammatory bowel disease. Click on the link below to complete the survey:
https://surveyswesternsydney.au1.qualtrics.com/jfe/form/SV_42el2fPpORED3Mi
Western Sydney University Human Research Ethics Committee Approval: H15913
Notice Of Annual General Meeting
Notice is given that an Annual General Meeting of the ACCA trading as Crohn’s & Colitis Australia (CCA) will be held online via video conference on Monday 27 May 2024 at 7pm AEST.
If you are a financial member of CCA attending the meeting or wish to provide an apology, please register online using the form below.
Please click the button below to download the notice of meeting, together with agenda and appendices.
Please enter your details below. Registered members who fill out this form will be contacted via email closer to the date of the AGM with the full meeting agenda and details of how to access the meeting via video conferencing.
Please note non-members will not be permitted to attend the meeting.
Registrations close 20 May 2024
2024 AGM Registration
For any enquiries regarding the AGM: 03 9815 1266 (option 0)
Sarah was told by a doctor, “I’ll eat my shoe if your three-year-old son has IBD”
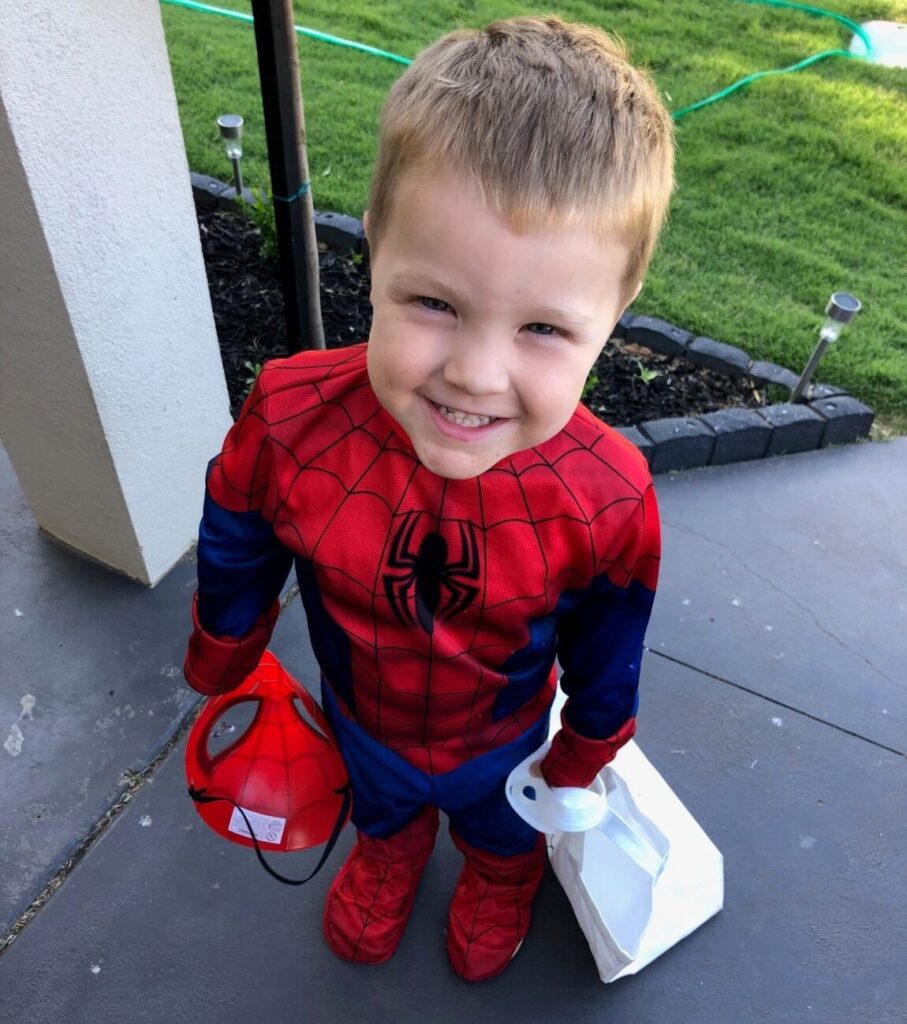
Recently, we sat down to talk with Sarah *, the mum of now four-year-old Chris *, who was diagnosed with IBD last year – when he was just three years old. Being diagnosed with IBD at such a young age is very rare. So rare, in fact, that before he was diagnosed, Sarah and her husband Charlie were told by one doctor that he would “eat his shoe” if Chris had IBD.
Not only is Sarah the mum of a toddler with IBD, but she’s also a nurse practicing within the paediatric healthcare system, so she has unique insight into what it means for young people to be diagnosed with and to live with IBD.
The diagnosis
Chris had what his parents knew were abnormal bowel movements for his whole life. Even the staff at Chris’ childcare facility flagged with Sarah that it was unusual how often he went to the toilet during the day.
Despite this, Chris didn’t show many other signs of having a chronic illness. Sarah says, “To this day, he’s never really looked like a sick kid. He’s always been a happy kid and had lots of energy, so in some ways it was difficult to imagine that there could be anything wrong with him. But, still, I just knew something wasn’t right.”
After initially living in Melbourne, the family moved to Swan Hill in rural Victoria. They had previously been told by doctors that Chris was just experiencing normal “toddler diarrhea”. It was shortly after the move when they noticed blood in Chris’ stool and Sarah and her husband both knew that something was wrong.
Even at this stage, doctors were sceptical that Chris could have IBD but his parents insisted on doing further tests and even paid to have a Calprotectin test done. When the results came back, Sarah recognised indicators of a potential chronic illness. From there, further tests were performed and Chris eventually received his diagnosis.
Sarah says, “In one way, we’re lucky because he’s really taken it in his stride. So many kids struggle with understanding why they have to take medicine every day or stick to certain routines, which of course is a very natural response for kids to have. It’s just never really seemed to bother Chris much. In another way though, that is a bit sad because I think it’s just all he’s ever really known. He doesn’t know any different, so he doesn’t complain.”
The treatment
When we spoke with Sarah, she informed us that they had just made the decision to escalate Chris’ treatment because he wasn’t having the response to the treatment that they had hoped.
“When we first received the diagnosis, there was an element of relief after knowing deep down for so long that something wasn’t right but not knowing what it was. Now, it feels like we’re facing a lot more uncertainty.”
Chris was started on the least invasive medication. However, he didn’t respond to it the way that doctors hoped. After continuing to have acute flare ups, he has had a couple rounds of steroids which is a good short-term solution but should be avoided where possible as a long-term treatment. It was suggested to Sarah and Charlie that Chris progress onto immunosuppressants- a step they decided to take in the last few days.
“Even being a paediatric nurse, the decision was so hard to make. It’s totally different when it’s your own kid. You have so much to weigh up and it feels like there’s a lot of uncertainty,” said Sarah.
Life with IBD
Chris’ parents are grateful that, so far, his IBD hasn’t been much of an interruption to his school or to him participating in all the normal activities that a four-year-old should get to enjoy. His diagnosis and treatment have meant that they often need to travel back and forth to Melbourne, something that they just accept now as part of their lives. They’re unsure of how IBD will continue to impact on Chris or how it will progress, but for now they’re taking it one step at a time.
Sarah says that if she could give parents in a similar position one piece of advice it would be, “Always trust your instincts. We have a great healthcare system and the doctors have done a great job but also, you know your kid better than anyone else in the world.
“Keep advocating for your kids and keep pushing for answers because there are crucial factors in these things that may not be easily visible to a doctor in an examination room or in a set of test results. I understand that not everyone will have the knowledge that I do when it comes to recognising signs in test results and things like that but as a parent, you have an intuition about your kids and their health that no one else does.”
To learn more about Crohn’s disease or to support the work of Crohn’s and Colitis Australia, which provides a wide range of programs and advice to those living with IBD, visit. https://crohnsandcolitis.org.au.
*names have been changed
A Crohn’s diagnosis at age 15: Aiyahna’s Story

Aiyahna’s journey with Crohn’s Disease began when she was just 15 years old. Unlike many Crohn’s sufferers (where finding an answer can sometimes take years), her diagnosis happened quickly following the discovery of a fistula that had tunnelled its way through the wall of her colon, as well as ulceration and inflammation throughout the entirety of her digestive tract.
Diagnosis
Aiyahna was fortunate to be diagnosed when she was, as a Gastroenterologist happened to be flying into her hometown of Longreach, Queensland. He performed a colonoscopy and upon seeing the results, he had her flown to Brisbane the following day to have further tests.
Prior to being diagnosed, Aiyahna experienced intermittent symptoms like mouth ulcers, exhaustion, occasional nausea, emotional overwhelm and digestive disturbances. Both Aiyahna and her parents chalked these up to being due to the stress of her transition into senior high school. Aiyahna says, “In hindsight, we weren’t wrong – as stress is most definitely an environmental trigger for Crohn’s episodes and symptoms – we just weren’t aware that an auto-immune disease was the underlying cause of those symptoms.”
Treatment
Following her diagnosis, Aiyahna had an extended stay in hospital, which was followed by two months of exclusive nasal gastric (NG) feeding. As a 15-year-old, already going through the trials and tribulations of adolescence, Aiyahna says having to feed herself through a tube was “pretty embarrassing and awkward at times” but that she was thankful for the support of her family, her school and her peers.
“I went to a small school in Longreach. Having already been through the isolation of COVID and a stay in hospital, I decided I wanted to go back to school despite having to feed myself through a tube. My school was very supportive. They gave me a key to the library, which had a kitchen where I could go and feed myself in privacy.”
Despite choosing to attend school during this period, Aiyahna could often only attend for half days as the fatigue of Crohn’s would overwhelm her. Not only that, but attending treatment sessions meant missing days of school at a time.
Aiyahna was treated through regular infliximab infusions (supported by daily medications) to help her body progress into remission. She continues with her infliximab infusion treatment regime four years on and is grateful to have maintained remission during this time. At the end of 2023, she was able to stop taking her daily medications.

Life with Crohn’s disease
When we asked Aiyahna what advice she would give to any young people living with IBD she said, “A lot of the time, we’re told that having IBD will be a barrier or that it will make things too hard. I don’t believe that. Yes, of course, things will be hard, but we can still achieve our dreams. It’s not about putting pressure on yourself, it’s just about being willing to give things a crack. And I actually believe that having Crohn’s Disease has taught me more than it’s taken away from me. I’ve become a stronger, more confident person because of it.”
This sense of optimism and determination is clear in Aiyahna. Even during our chat, she’s in her uni library studying. Despite the extensive interruptions to her education and the challenges she’s faced over the last few years, she has moved to Brisbane where she’s studying at the University of Queensland to become a psychologist.
Aiyahna is grateful for the support she has had from her family throughout her diagnosis. When her mum spoke about the challenges of her daughter being diagnosed with Crohn’s Disease, she said, “I realised that it was not my job to clear the obstacles for her, to smooth her path, nor to give her the answers but rather, my job was to guide her to look for the possibilities within the struggle, to remind her to focus on her strengths and to use them to negotiate the obstacles she encounters.”
In June 2023, Aiyahna transitioned from the paediatric healthcare system into the adult healthcare system. She’s currently in conversation with her doctor about switching to self-injections for her infliximab and says the transition has given her more decision-making control over her treatment plan and ultimately more flexibility and independence in her life.
Aiyahna says, “Living with Crohn’s can feel like riding a rollercoaster at times. Starting with a huge uphill climb as our bodies recover, followed by enormous drops as we realise that our lives have to change, moments when we feel like we are flying upwards as we regain momentum in life and then those moments of coasting as we adjust to our new normal. However, I have found that around every corner there is a lesson learned and a strength found, empowering us from within and shaping the people we are yet to become.”
To learn more about Crohn’s disease or to support the work of Crohn’s and Colitis Australia, which provides a wide range of programs and advice to those living with IBD, visit https://crohnsandcolitis.org.au.
Research reveals that young people with IBD aren’t receiving the care they need.
Australia, 1 May 2024 – Research has highlighted gaps in the paediatric healthcare system for young people living with Inflammatory Bowel Diseases (IBD). This is why the focus of this year’s Crohn’s and Colitis Awareness Month- which is May – is the impact of IBD on young people.
The results from the Inflammatory Bowel Disease Paediatric Quality of Care Patient Experience Survey 2023 highlighted concerning issues in a number of areas but most concerningly, mental health, delay in diagnosis and treatment access:
- Mental Health: IBD can impose a profound psychological burden on young people
Young people with IBD have more than a 50% risk of developing mood or anxiety disorder. Despite this, the survey results identify access to mental health support as being problematic.
Over half the young people surveyed, reported no query about their mental health from any health professional in the past year (62.4%); and less than a third that accessed mental health support felt it was easy to do so (29.7%). Additionally, accessible mental health support was the most common suggestion for improved IBD care.
- Delay in diagnosis and access to prompt advice, specialist review, and procedures
Waiting times for specialist review of a suspected disease relapse surpassed the national standard of five days for around half of respondents (49.8%), often exceeding two weeks (26.8%).
People often sought private services such as radiology and colonoscopy/surgery services to avoid treatment delay (85.1% and 79.3%). Uncertainty or an outright lack of access to prompt advice via an email or phone helpline was common (23.7%).
- Care is not being tailored to the needs of young people
More than a third of young people (38.3%) aren’t being referred to a paediatric gastroenterologist upon first suspicion of IBD. The results also showed that information and educational opportunities are more often afforded to ang geared towards adults rather than youth.
Associate Professor Ed Giles, Chair, IBD Paediatric Quality of Care Project Advisory Committee, says there are issues that need to be addressed within the healthcare system when it comes to the quality of care that young people with IBD are receiving.
“While it’s encouraging to see improvements in some areas of care for young people who are either in the process of being diagnosed with IBD or who have already been diagnosed, it’s also concerning to see a regression in other areas.”
“We’re seeing gaps in healthcare infrastructure when it comes to dealing with the psychological impact that IBD can have on young people as well as increased barriers when it comes to accessing services, getting educated and being able to receive a diagnosis. The report also shows that young people in rural and regional areas are more likely to be impacted by these gaps in the system.
“If we take action on the information provided in these reports, we can make a real impact on the lives of young people living with IBD,” Associate Professor Giles said.
CCA recently interviewed Aiyahna, a young person with IBD and Sarah, the mum of a four year old boy who was diagnosed with IBD at the age of three. Their stories reflect the reality of what the latest research tells us.
Aiyahna spoke about the mental resilience required when living with IBD.
“Living with Crohn’s can feel like riding a rollercoaster at times. Starting with a huge uphill climb as our bodies recover, followed by enormous drops as we realise that our lives have to change, moments when we feel like we are flying upwards as we regain momentum in life and then those moments of coasting as we adjust to our new normal. However, I have found that around every corner there is a lesson learned and a strength found,” Aiyahna said.
Sarah is a paediatric nurse who lives with her family in rural Victoria and was told by one doctor that he would “eat his shoe” if her son had IBD. She spoke about the difficulties and the delay in receiving a diagnosis for her son and the scepticism she faced from doctors.
“Keep advocating for your kids and keep pushing for answers because there are crucial factors in these things that may not be easily visible to a doctor in an examination room or in a set of test results. As a parent, you have an intuition about your kids and their health,” Sarah said.
To read more about Aiyahna’s and Sarah and Chris’s stories, you can visit: News – Crohn’s & Colitis Australia (CCA) (crohnsandcolitis.org.au)
CCA acknowledges and thanks our generous sponsors, Pfizer, Johnson & Johnson, Dr Falk Pharma, Celltrion, Takeda and AbbVie.
For media enquiries contact Tiarna Adams 0478 074 288 or [email protected].
ABOUT CROHN’S & COLITIS AUSTRALIA
Crohn’s & Colitis Australia (CCA) has been working with people living with Crohn’s disease and ulcerative colitis, healthcare professionals, governments and the public to minimise the impact that these conditions have on the community since 1985. In that time, CCA has been the only Australian organisation working with and for patients and their families, the doctors that treat them, and the policymakers who can bring about change. CCA provides high quality information, supports life-changing research and campaigns vigorously – for more knowledge, better services and more support for people affected by inflammatory bowel disease. For more information, visit: https://www.crohnsandcolitis.org.au/
When I was 17 and still living in the UK, I had an upset stomach and started experiencing what I now know are symptoms of IBD – including blood in my stool, weight loss and an urgent need to go to the toilet with extreme regularity. I was told I had a stomach bug and that it would pass. Fast forward a couple of months where I wasn’t getting better, and – at the urging of my dad – I managed to get an appointment for a flexible sigmoidoscopy.
I vividly remember – I was lying in my hospital bed. I just came out of the scope, and a lovely nurse spoke to me and gave me like a printout about ulcerative colitis (UC). Then I saw a consultant a couple of weeks later and received the official diagnosis. At that time, I was very confused. I didn’t know what this illness was, or what it meant. I started doing my own research and kind of went from there, but I truly felt like I was the only person who had this condition. I felt very lonely and isolated — it was a lot to take in as a young person. My IBD nurses and close friends were fantastic in helping me get through this, but I think it’s relatively easy when you’re first diagnosed to exclusively focus on your physical wellbeing. As a consequence, I think it can be easy to neglect your mental wellbeing. I would strongly encourage others who are diagnosed to speak to somebody about what they are feeling and going through.


Following the diagnosis, I found social media to be a powerful tool in connecting with other people living with IBD. This was important for me in feeling less alone. I remember following this person on Instagram with ulcerative colitis, and experiencing a feeling of, “wow. Somebody has my illness.” Then, I explored the hashtags, and identified that quite a few people shared my condition. I created my own account – @ibdlottie – to share what I was going through. I have now developed a strong community and support network, and have made really good friends. Some of these relationships exist online, and I’ve met up with people in person due to this connection. Especially following my move from the UK to Australia, this community has been really important.
I’m not currently flaring, but I still have what I call ‘mini flare ups’. I’ll go through two or three days where I feel unwell, before recovering. I find that I do get quite tired and worn out, and I experience cramping and sore joints quite a bit. It can also take me longer to recover from illnesses, and there are certain foods that I can’t eat. I’m 24 now and I was diagnosed when I was 17. As such, it’s difficult for me to remember what my “normal” was. I sometimes get in my head, and am unsure as to whether I’m feeling a certain way because of my UC or not.
From a mental health perspective, talking to others about your experience has been so helpful in reducing feelings of isolation. After moving to Australia at the end of last year, I’ve had people message and say, “I didn’t know if I could travel with IBD, but seeing you do it has made me realise that I can do it.” My UC has also encouraged me to live in the moment, and to live to the fullest, particularly while I’m feeling well. For instance, I’m not sure I would’ve run a half marathon, or moved to Australia, if not for this attitude.
There’ll be good days and bad days, but I know that there’ll be opportunities to do things that challenge and excite me, and I’ll take on that opportunity whenever I can.
To share your story, click here.
Survey on the sexual and reproductive health needs of women in Australia with IBD
Researchers at Western Sydney University and Auckland University of Technology want to
understand what the sexual and reproductive health needs are of women who live in Australia with
the chronic condition of Inflammatory Bowel Disease.
If you have a diagnosis of Inflammatory Bowel Disease, and would like to have your voice heard,
please contact the research team at Western Sydney University using the email address:
[email protected]
Any information you provide will be treated confidentially and will be used to inform strategies that
enhance awareness about the sexual and reproductive health issues associated with inflammatory
bowel disease.
Click below to complete the survey:
https://surveyswesternsydney.au1.qualtrics.com/jfe/form/SV_42el2fPpORED3Mi
Inspiring others and raising awareness: Tahlia’s story

I was diagnosed with Ulcerative Colitis at the age of 21 during the COVID pandemic after having symptoms of tiredness, diarrhea and multiple flare ups.
Since my diagnosis I have trialled many different treatments and medicines which have included prednisolone, pentasa, mercaptopurine and Vedalizamab. I am now on Infliximab infusions which I have every six weeks at my local hospital which has now put me in remission along with my other medicines.
I also have to have yearly colonoscopy to see how I am progressing with this disease, and have a great support network which includes family, friends, nurses and doctors.
When I am in a flare up I cannot leave home which makes me feel frustrated and isolated from family and friends. I had to find an alternative for work, so I started working from home.
When my flare up is under control, I am able to do some volunteer work and am able to go in to work. I also like to try and exercise and catch up with friends.
I am hoping my story will inspire others and raise awareness for this disease.
To share your story, click here.

Hi There! My name is Aiyahna and I am an 18-year old Crohn’s Disease Warrior.
My Crohn’s story began a mere three years ago when I was 15 years old. Unlike most Crohn’s disease sufferers (whose diagnosis can sometimes take years), my diagnosis was swift due to the discovery of a fistula (that had tunnelled its way through the wall of my colon) in addition to ulceration and inflammation throughout the entirety of my digestive tract. After an extended hospital stay, my initial Crohn’s treatment featured two months of exclusive nasal gastric (NG) feeding (to assist in soothing and reducing inflammation within my digestive system), followed by a cautious re-introduction of nutrition adhering to a strict Crohn’s diet (gluten, dairy and preservative/additive free). During this time, I was also treated through regular infliximab infusions (supported by daily medications) to help my body progress into remission. I continue with my infliximab infusion treatment regime 3 years on and am grateful and fortunate to have maintained remission during this time.
Prior to my initial acute flare, I was unaware that my own body was attacking itself and ravaging the inside of my body. We (my family and I) had thought the symptoms I had been intermittently experiencing – mouth ulcers, exhaustion, occasional nausea, emotional overwhelm and digestive disturbances – were physiological responses to the stress of my transition into senior high school. In hindsight, we weren’t wrong – as stress is most definitely an environmental trigger for Crohn’s episodes/symptoms – but we were just not aware that an auto-immune disease was the underlying cause of those symptoms.
Living with Crohn’s can feel like riding a roller-coaster at times. Starting with a huge uphill climb as our bodies recover, followed by enormous drops as we realise that our lives have to change. Moments when we feel like we are flying upwards as we regain momentum in life, and then moments of coasting as we adjust to our new normal. Then comes all the twists and turns, loop-de-loops and upside-down moments as we go to battle for our body and remember the ease of life pre-Crohn’s. However, I have found that around every corner there is a lesson learned and a strength found, empowering us from within and shaping the people we are yet to become. The best thing about this Crohn’s journey, like with most rollercoasters, is that all the challenges faced—those scary, heavy moments where all you want to do is get off the ride— are what brings us to the moments that makes us feel most alive. It’s a gift showing us just how wonderful it is to live —knowing pain and discomfort and still choosing to show up and find the good, regardless.

My Crohn’s story is not just about Crohn’s; nor is it just about my diagnosis, my physical health or my recovery and current remission status.
My Crohn’s story is one of acceptance. I live with Crohn’s but am not defined by it nor controlled by it.
My Crohn’s story is one of creating opportunity from within my experiences rather than limiting myself.
My Crohn’s story is not one of self-pity, nor is it a story about excuses or reasons to give less than my best. It is not about dwelling upon the unfairness of my body being home to a disease. Rather it is an encouragement for me to be a little more respectful of my body’s uniqueness and to live a full and vibrant life that nurtures my health.
My Crohn’s story is both a promise and a reminder to myself, and in shared camaraderie with our IBD community. A promise to myself that I can choose to thrive, and a reminder that my thoughts, my attitude and the ownership of my choices will be the difference between suffering through IBD, and growing and thriving with IBD.
My participation within the Crohn’s and Colitis Australia Youth Empowerment Program (YEP) reflects my promise. When I was diagnosed in 2019, Crohn’s and the world of IBD were foreign to us (myself and my family). We found it difficult to source reliable information to help us to understand the disease – from diagnosis, to treatment, to prognosis. We also found it difficult to access ‘age-appropriate’ support (outside of my Gastroenterologist) to navigate the process from illness to remission and all the wild, roller coaster, moments in between. I found myself feeling a little disconnected from my peers, somewhat isolated, a little alone and a lot unsure of myself. Our family has a saying, “You can’t do it alone, but only you alone can do it.”

As IBD sufferers, we need to take personal responsibility for helping our bodies to support our health. However, you do not need to be alone in your journey. Seeking and accepting support will be critical in helping you to manage your disease and to find answers, new information and ideas. You will be supported by your doctors, your family and, if you allow them to, your friends and your community—including all of us here at “YEP! Online”. We’re all here with you on your journey— we want you to share in our enthusiastic and positive camaraderie and we want you to know that you’re not alone!
So, welcome to the greatest journey of your life. Crohn’s is not a test (though it may feel like one sometimes)—it is an opportunity for you to discover just how amazing your body is and to uncover the hidden depths of strength inside of you. We have a magnificent opportunity to teach others around us how to flourish — regardless of their circumstances or the challenges we are facing. So, let’s do this together. Let’s build a team, let’s support each other, let’s lift each other up and let’s make a difference. Let’s make our life stories —despite living with IBD – extend beyond the ordinary. Instead, let’s make them extraordinary!
To share your story, click here.

Sleep is a part of our everyday life and an essential process for maintaining overall health. When we sleep our body can regenerate and repair itself. Poor sleep is associated with worse overall health and can even increase the amount of inflammation in the body. What is more, our sleeping patterns can influence the functioning of our gastrointestinal system. IBD, with its alternating remissions and relapses, results in a variety of symptoms among which poor sleeping patterns are a common one. Although the potential impact of the medications used for treating IBD on sleep has been investigated, the assumed relationship, has not been clearly established.
An Australian study published in 2023 demonstrated that the medications used to treat IBD can be associated with sleep quality. The study involved answering an online survey and included a total of 544 respondents. Common medications that participants were taking included opioids, vitamin D, corticosteroids, methotrexate, and biological agents such as Humira.
Opioid use in the general population is a recognised factor contributing to poor sleep particularly due to sleep apnoea, an associated condition causing uncontrollable pauses in breathing. The study has shown that opioid use was correlated with the long-term IBD history and a high severity of the condition. Other studies have already demonstrated that opioid use in people with IBD was linked with poor quality of life.
Infliximab and vitamin D were also found to be linked with poorer sleep but patients taking them had on average a higher body weight. High body weight is associated with poorer sleep in the general population due to increased risk of sleep apnoea.
Corticosteroids can cause problems with sleep and should generally be taken in the morning. In this study it was difficult to assess the link between corticosteroids and sleep. The fact that corticosteroids are used to treat more complex IBD and their known impact on mental health of the patients might have a confounding effect.
Methotrexate has a known link with fatigue, and in this study only a limited number of participants were treated with this medication (8%). Therefore, the researchers were unable to identify any link between methotrexate and sleep quality. However, some previous studies reported such a correlation.
Despite the study potential limitation (an online questionnaire could attract people with sleeping problems), it increases our understanding of the associations between the use of certain medications and sleep in IBD. Of course, further research is recommended to recognise and document the relationship between sleep quality of IBD patients and their medication use. As the studies available to date are correlational, we cannot be certain of the causal relationship between sleep quality and IBD course.
If you would like to know more about sleep and IBD please follow the link:
The studies mentioned in this article could not have been possible without the contribution of hundreds of people with IBD. IBD research is an active area, and you can be a part of it by participating in one of the active studies here.
Ingredients
- 9g instant stock powder or 3 whole cubes dissolved in 3 ½ cups hot water
- ½ tsp Chinese five spice
- 2 tbsp soy sauce
- 2 tbsp fresh coriander chopped
- 300g carrot, peeled and cut into matchsticks
- 300g parsnip, peeled and cut into matchsticks
- 2 celery sticks, trimmed and cut into matchsticks
- 200g Bok choy finely shredded
Method
- Bring stock to boil in a large saucepan over high heat
- Add Chinese Five Spice and cook 2-3 minutes
- Reduce heat to low, add soy sauce, coriander and vegetables. Cook for 5 minutes. Season with salt and pepper if desired, and serve in a warm bowl
Can be served as a meal by adding 125g flat rice noodles or 120g cooked prawns/chicken meat.
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
Chicken & leek casserole
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
Serves 4
An easy recipe for your slow cooker!
Ingredients
- 4 skinless chicken breasts
- 2 onions, peeled & sliced
- 1 garlic clove, crushed
- 2 carrots, thinly sliced
- 2 leeks, trimmed & sliced
- 400g tin chopped tomatoes
- 570ml chicken stock
- Pinch of thyme
- Salt & freshly ground peopper
Method
- Add all ingredients, diced into your slow cooker.
- Cook on low for 6-8 hours.
- Thirty minutes before serving, stir in corn flour and simmer.
As always: if any of these ingredients are flare foods for you, please omit them or replace them with an alternative item.
Submitted by Nicola Allsop