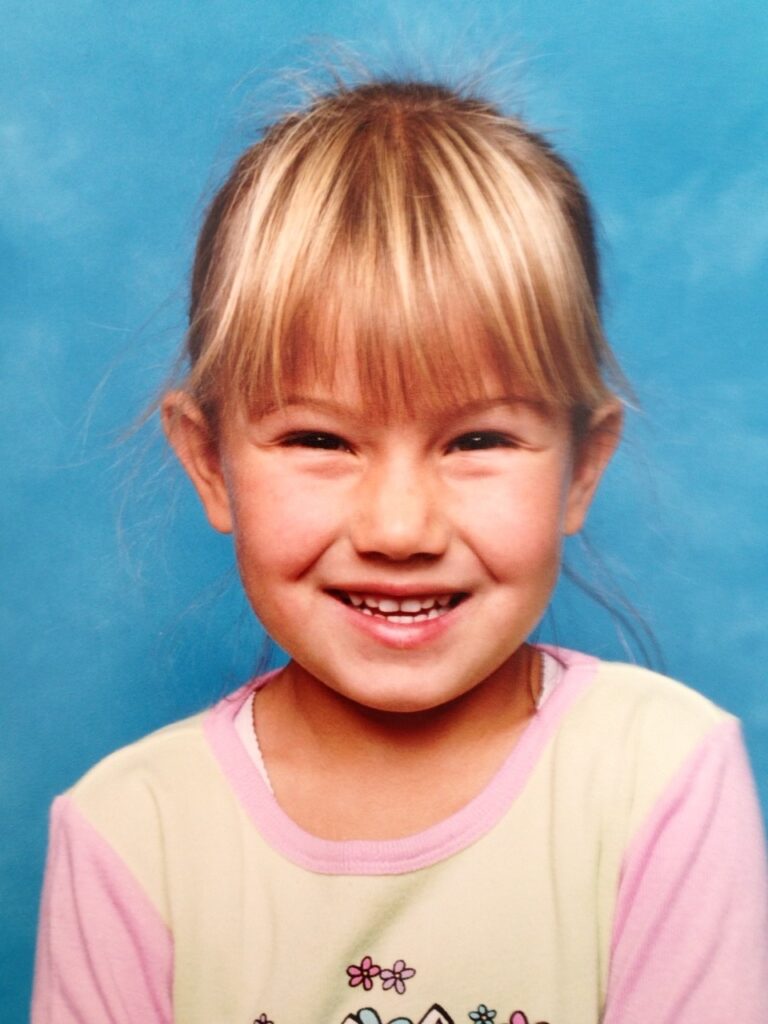
Food fight: Charlotte’s Story

I’ve always been a healthy person. I played sports, exercised, and ate right. But when I was 16, I was taken to the hospital with severe stomach pains, and they diagnosed me with pancreatitis. Since then, doctors told me it made no sense that I would have pancreatitis because it is very uncommon in teenagers. I never understood why I received that diagnosis.
It wasn’t until 2017, when I was 21, that I found out the truth about my condition: Crohn’s disease. After a trip to Bali, I noticed blood in my stools. I consulted a doctor and, embarrassingly, asked my male doctor if I had a parasite or if blood was normal. Next thing I knew, I was up on the table with two female nurses observing while my doctor checked for hemorrhoids. I was mortified. Little did I know this would become a regular routine at the doctor’s office! A colonoscopy was scheduled for the following week, which confirmed severe Crohn’s disease.
After being diagnosed with Crohn’s disease, I didn’t know my diet would be an important part of my treatment. Before IBD, I assumed that bloating was naturally associated with certain foods, so when I started experiencing lots of bloating, I assumed it was normal. Gluten is the main culprit for a lot of my bloating, and early on in my diet journey, the variety of gluten-free foods was limited. And if there were choices, they weren’t very good!
For the first three years after my diagnosis, I was very strict with my FODMAP and gluten-free diet. I’m a foodie, so this was tough. My poor taste buds and bank account suffered! Gluten-free food often tasted like cardboard and would fall apart in your hand.

Despite the difficulty of finding foods that fit within my dietary restrictions, there were upsides. It forced me to get creative in the kitchen, and now I’m a better cook than ever! I had to learn how to cook my own meals from scratch, which didn’t bother me initially, but it became monotonous. I felt like I was missing out on special occasions with friends because I couldn’t indulge in the same food, and I feared restaurants wouldn’t cater to me.
During my worst flare-up, I had a negative mindset about my diet after I stopped responding to my medication and steroids. I started eating whatever I wanted, thinking, “Well, it couldn’t get any worse.” But it did, dramatically! I didn’t realize how crucial my IBD diet was for staying on track and keeping inflammation minimal. It took a long time to gain control of my diet, and I received help from my specialists. Now, with their supervision and a dietitian, I’m working on reintroducing different foods into my diet now that I’m receiving the right treatment. But life is too short not to indulge sometimes!
I’ve made up a term for my approach: the nine-out-of-ten rule. Nine out of ten times, I stick to my FODMAP-free and gluten-free diet, but occasionally, I will have a piece of birthday cake or some cheese with my friends. I call this the optional diet, which works for me because it helps me enjoy life without feeling guilty or limiting myself because of this disease. This optional diet does come with consequences, but sometimes I really needed to put my happiness first.
I’ve made significant changes to my diet, primarily cutting out foods that caused me discomfort and bloating. I stopped drinking coffee first thing in the morning and reduced my meal sizes, opting instead to eat more frequently throughout the day and consume more fiber.
Keeping a food diary has been incredibly helpful, especially when I first started or when I notice I’m entering a flare. It encourages me to track what I eat (and how it made me feel), which helps my dietitian and me figure out which foods I’m reacting to the most, even if they’re FODMAP- or gluten-free-friendly.
When I began my new diet, one of the biggest challenges was incorporating it into my daily life. I wanted to enjoy my meals and not feel like I was missing out. When I first started shopping for gluten-free products, I spent hours in the supermarket reading the back of labels. I would spend an hour at Woolworths, then an hour at Coles, and end up at the butcher or local farmer’s markets.
Many products in the supermarkets are gluten-free but not located in the health food aisle, and their packaging isn’t always obvious if you don’t know what to look for.
One strategy that helped me was treating grocery shopping as an outing. Every week, I go to the Dandenong Market or Costco if my local farmer’s market is closed, and I go with my neighbor. We could have lunch or coffee before shopping, making the experience stress-free and more enjoyable. FODMAP and gluten-free food shopping can become overwhelming. Now that things are looking up again, you’ll find me in front of the oven or reading recipes for some new and exciting dishes every night!
The key to making great meals is learning how to substitute foods, especially if you have dietary restrictions like mine. Understanding how many food products contain wheat was mind-blowing at first. It was challenging, but I learned quickly to do my homework before buying anything packaged or pre-made.
I enjoy making different salads with protein, but finding dressings without garlic, onion, and gluten-free and dairy-free ingredients was a struggle. When you Google “salad dressings” with those criteria, the search still returns dressings containing all the ingredients you can’t eat! This is dangerous, especially for someone who is trusting of internet information. I found this frustrating, so I started making homemade dressings myself.
I’m a huge advocate for healthy, organic, and gluten-free eating, but it can be expensive. Planning is key! I plan all my meals for the week and create detailed grocery lists so I know where I’m going and what I need to purchase. It was super hard being a university student with a mortgage, juggling a social life, paying for medication, and living away from home.
Tips that have worked for me:
- Replacement garlic and onion powders from the FODMAP store are a game-changer when cooking at home. I use them almost every night, and my partner can’t tell the difference from regular garlic and the replacement powder.
- FODMAP phone app: This life-saving app gives you traffic light indicators on which foods are triggering and how much of a certain food is safely tolerated by most people with IBS symptoms before the intake should be avoided. It’s helpful for family members wanting to avoid triggering me! My mom uses the app when we have family meals to know which foods to cook.
- Gluten-free bread: I’ve tried almost every brand out there, and Aldi’s gluten-free bread is the best. It stays soft and doesn’t crumble easily, which is what you want from a good loaf. The pieces are decent and thick enough to make a sandwich. Second place goes to Woolworths’ home brand English muffins.
- Breadcrumbs: Woolworths Homebrand breadcrumbs are by far the best. They are located in the health aisle. I wish someone had told me this!
To learn more about IBD and Nutrition, visit here.
First published in CCA’s Insight Magazine 2023 edition