Optimising bone health in IBD
Key points
- Inflammatory bowel disease (IBD) increases the risk of osteopaenia and osteoporosis.
- Osteoporosis makes bones weak and more easily broken.
- Eating enough calcium, Vitamin D and doing exercise can protect bones.

This dietary resource developed by GI DREAM provides general dietary information on optimising bone health with Inflammatory Bowel Disease (IBD).
Why is bone health important in IBD?
Bones have many important functions in the human body including forming our skeleton, creating red and white blood cells and acting as a storage bank for minerals. Individuals with IBD are at increased risk of low bone mass; termed osteopaenia or osteoporosis.
What is osteopaenia/osteoporosis?
Osteoporosis refers to a loss in bone mineral density which causes weaker, more fragile bones that have an increased risk of breaking. Osteopenia is a reduction in bone mass that is less severe than osteoporosis but is considered a risk factor to developing osteoporosis. Up to half of IBD patients have osteopenia or osteoporosis. Post-menopausal women with IBD also have a higher risk of developing osteoporosis.
Osteoporosis can lead to:
- Increased risk of fractures
- Back pain
- Stooped posture and loss of height
- Reduced ability to carry out daily activities if mobility is affected.
What can increase the risk of osteoporosis in IBD?
- Decreased absorption of calcium and vitamin D caused by inflammation in the small bowel.
- Not eating enough calcium. Calcium helps keep our bones strong and they require a regular supply. If we do not consume enough calcium, the body takes it from our bones, making them weaker and more likely to break.
- Having a low Vitamin D level. Vitamin D is essential for maximising absorption of calcium from the foods we eat and helps our body build bone mass with calcium.
- Reduced ability for bone formation during periods of inflammation
- Low body weight and not eating enough protein due to poor appetite and reduced food intake caused by symptoms of IBD
- Long term use of steroid medications can reduce bone formation, increase bone breakdown and reduce calcium absorption
- Low physical activity levels – specifically weight bearing activity, as this exercise is great for maintaining bone health and muscle strength.
How is osteoporosis screened for and detected?
Bone mineral density is assessed by a specific X-ray called Dual-energy X-ray absorptiometry or “DEXA” that examines the density of the bones at the hip and spine.
How can I prevent or manage osteoporosis?
- Eat a healthy, balanced diet with enough calcium and protein rich foods.
- Get enough vitamin D from sunlight. Usually, most people can meet vitamin D recommendations with adequate sunlight exposure. Discuss with your gastroenterologist as some IBD medications require caution sunlight exposure.
- Weight-bearing exercise. Being active every day is important. Aiming for 150-300 minutes per week of moderate intensity exercise is recommended for general physical health. To optimise bone health, weight-bearing exercise is recommended. This includes hill-walking, jogging, dancing and/or resistance training using free weights and resistance bands.

How much calcium, vitamin D and protein do I need?
Calcium
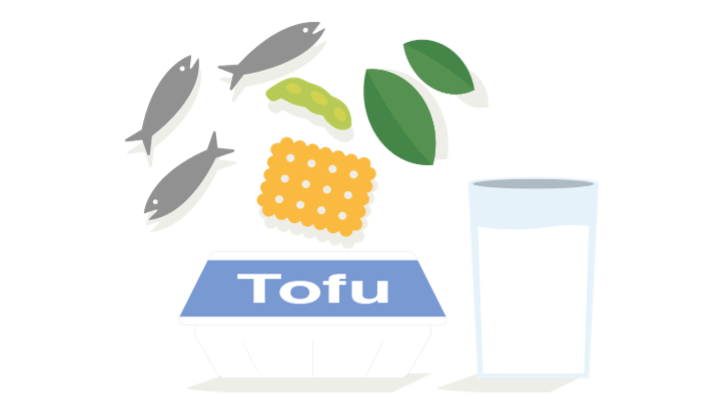
Calcium is mineral found mainly in dairy foods such as milk, yoghurt and cheese. It can also be found in bones of fish, soy foods and fortified products (e.g. tofu, cereals, nut or oat milk). If you are at risk of osteoporosis or have osteoporosis, include more calcium rich foods into your diet.
| Age group(s) | Calcium requirements |
|---|---|
| Men | Per day |
| 19-50 years old | 1000mg |
| 51-70 years old | 1000mg |
| > 70 years old | 1300mg |
| Women | Per day |
| 19-50 years old | 1000mg |
| 51-70 years old | 1300mg |
| > 70 years old | 1300mg |
Other tips to boost calcium in your meals:
- Calcium from animal-based foods is better absorbed than calcium from plant-based sources.
- If using dairy alternatives ensure products are fortified with calcium at least 100mg/100ml.
- Grate cheese over salads, soups or pasta.
- Eat cheese/sardines/tinned fish containing bone on toast.
- Add 1-2 tablespoon skim milk powder to creamy soup.
- Add almonds to yoghurts, salads, snacks.
- Add tofu and Bok-choy to stir-fries, noodle and rice dishes.
- Add Greek yoghurt to curries.
- Have pita bread/crackers with tzatziki/cheese.

| Calcium rich foods | Serving size | Calcium |
|---|---|---|
| Animal-based sources | ||
| Canned sardines with bones | 90g | 342mg |
| Yoghurt | 200g | 330mg |
| Skim milk powder | 25g | 312mg |
| Low fat milk | 250ml | 340mg |
| Canned salmon with bones | 95g | 211mg |
| Parmesan cheese | 20g | 194mg |
| Swiss cheese | 20g / 1 slice | 177mg |
| Cheddar cheese | 20g / 1 slice | 113mg |
| Plant-based sources | ||
| Firm tofu | 100g | 320mg |
| Soybean milk, fortified | 250ml | 296mg |
| Breakfast cereal, fortified | 30g | ~80-200mg |
| Milo cereal | 30g | 200mg |
| Almonds | 30g | 75mg |
| Bok-choy, cooked | 0.5 cup | 65mg |
Vitamin D
You can also include foods high in vitamin D to boost your vitamin D intake. Some sources of vitamin D are fatty fish (salmon, tuna, and mackerel), eggs, fortified spreads and some margarines. Some research also shows that leaving mushrooms in the sun for 10-20 minutes can boost their vitamin D content to 100% of your daily needs (in ~8 mushrooms).
If your vitamin D levels are low, your doctor or dietitian can provide advice on whether vitamin D supplementation is required. Speak to your GP on how to best manage your vitamin D levels.
| Age group(s) | Vitamin D |
|---|---|
| Men | Per day |
| 19-70 years old | 5.0μg |
| 51-70 years old | 10.0μg |
| > 70 years old | 15.0μg |
| Women | Per day |
| 19-50 years old | 5.0μg |
| 51-70 years old | 10.0μg |
| > 70 years old | 15.0μg |
Protein
Not eating enough protein can impair bone growth. Most Australians eat more protein than they need, but people with IBD (especially during flares) may not if their diet is limited by symptoms or food restrictions. This can lead to weight loss and, in some people, long term low body weight which increases the risk of osteoporosis.
Good sources of protein include lean meat, fish, dairy, whole grains, legumes, tofu, eggs and nuts. For further information refer to Nutrition for IBD.
Find an IBD dietitian to speak with if you are concerned about your protein intake, are restricting your diet or have lost weight without trying.
Acknowledgements:
This resource was developed in 2022 by the DECCAN Education Materials Working Group and reviewed by the GI DREAM Board in line with ECCO Consensus on Dietary Management of IBD (2025). Requests and enquiries about this document should be directed to [email protected] or website www.gidream.org. GI DREAM does not take any liability for any injury, loss or damage incurred by the use or reliance on this information. Reviewed August 2025. Date for review August 2027.