Colonoscopy
Key points
- A colonoscopy is a procedure in which a long, flexible tube is inserted into the rectum and steered around the large bowel (colon). The tube has video technology to allow the lining of the bowel to be examined in detail
- You may be advised to have a colonoscopy to diagnose Crohn’s or colitis, monitor whether your IBD treatment is working, or to check the bowel for abnormalities that could lead to cancer
- You will need to take a bowel preparation medication to ensure the bowel is empty before the procedure. This makes the colonoscopy easier to perform, improves the doctor’s view, and makes it safer
- A colonoscopy is generally a very safe procedure with minimal risks
What is a colonoscopy?
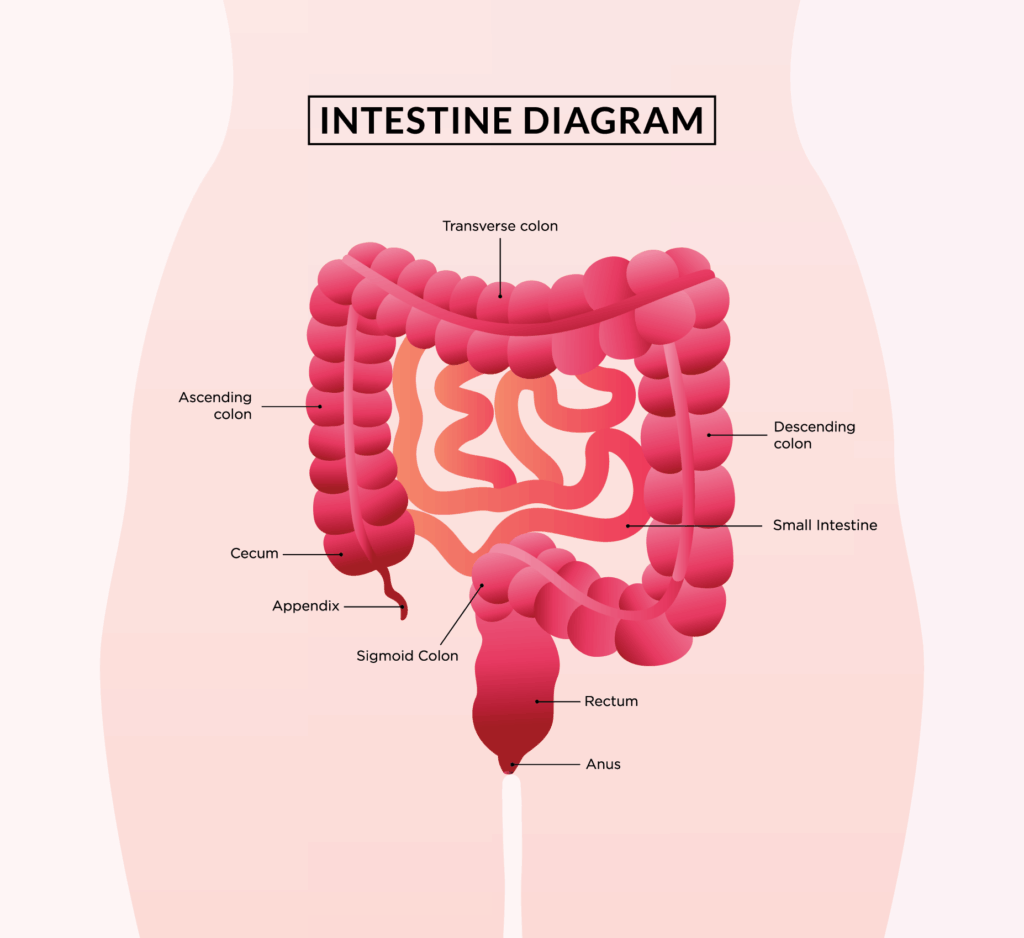
A colonoscopy is a procedure that involves a long, flexible tube with a light and video camera at the end being gently inserted into the rectum and guided through the colon.
Through the video technology, the specialist can view the entire inner lining of the large intestine and identify any areas of concern, such as inflammation (which could be Crohn’s or ulcerative colitis), polyps (pre-cancerous growths), or abnormal tissue that could be cancerous. The specialist may also take tissue samples (biopsies) to investigate abnormalities or to help understand the cause of bowel symptoms.
Colonoscopies are typically done under sedation, so you should be relaxed and comfortable without any pain during the procedure.
Why do I need a colonoscopy?
There are a range of reasons you might need a colonoscopy:
- To diagnose disease. A colonoscopy can help to diagnose the type of inflammatory bowel disease (IBD) you have and assess the extent and location of inflammation. It can also help your specialist detect polyps or suspicious growths that may indicate bowel cancer. Polyps are usually removed during the procedure and any tissue samples can be sent to the lab for analysis.
- To monitor treatment. Colonoscopies can assess whether inflammation has improved after changes in IBD treatment, such as adjusting medication doses or starting a new therapy. However, recent advancements have made non-invasive monitoring options more common, including faecal calprotectin to assess inflammation (measured through a stool test), magnetic resonance imaging (MRI) and intestinal ultrasound. You can speak to your specialist to understand which monitoring option is most suitable for you.
- For disease prevention. Colonoscopy is also used for bowel cancer screening and can help to detect early changes in the bowel lining before cancer develops.
To have a colonoscopy, you need a referral from your GP or gastroenterologist.
How often should I get a colonoscopy?
How often you need a colonoscopy depends on your individual health and medical history and your specialist will explain the right schedule for you. Typically, people living with IBD are recommended to have a colonoscopy every 1-3 years (or longer in some circumstances) to monitor treatment, screen for abnormalities, and help prevent bowel cancer. This should happen even if your IBD symptoms are well controlled.
What will I need to do?
Before your colonoscopy, your bowel needs to be completely empty. It’s important to follow the instructions provided by your specialist carefully. Make sure you ask any questions you have so that you feel comfortable going into the procedure.
A few days before the procedure, you may be advised to follow a low-fibre (referred to as low residue) diet. This diet generally avoids wholegrains, nuts, seeds, dried fruit, and raw fruits and vegetables. Foods such as white bread, refined breakfast cereals, meat, and dairy foods are usually allowed. Following this diet helps ensure the bowel preparation works effectively so your specialist can clearly see the bowel lining during the procedure.
You may also be asked to stop certain supplements, such as iron, before the procedure. Always ask your specialist for personalised advice about your medications and supplements, and if and when to stop taking them.
You will also need to take a bowel preparation medication (bowel prep) as advised by your doctor or gastroenterologist. This is usually started the day before the test and contains a laxative that will cause you to have watery diarrhoea to help empty your bowel. Make sure you plan ahead to ensure you can stay close to a toilet during this time.
After starting the bowel prep medication, you will need to switch your diet to clear liquids only. For example, clear broth, apple juice, black coffee or tea, and clear sports drinks. Keep your liquid intake high, even if you don’t feel thirsty. By the end of the bowel preparation, your poo should be liquid, clear or light yellow in colour, and free of any solid particles.
On the morning of the procedure, you won’t be able to eat any solid foods and will usually need to stop consuming all liquids (even water) several hours beforehand.
The exact process differs between people and the type of bowel prep medication you have, so make sure you follow the instructions that were given to you. This will ensure your bowel is completely empty and you don’t have to get the test re-done.
Tips to make the bowel preparation more comfortable
Bowel preparation isn’t pleasant, but it’s very important for a successful procedure. The Crohn’s & Colitis Australia community sent in some tips that have helped them with the bowel preparation:
- Make sure the prep is cold when you drink it
- Drink the prep from a cup with a straw
- Drink other clear liquids in between to get rid of the taste and stay hydrated (e.g. apple juice or clear Gatorade)
- Eat lemonade icy poles to satisfy the urge of eating something without affecting the preparation
- Drink hot (clear) broth to ease nausea and feel more nourished
- Apply Vaseline around the anal area before your first bowel motion and in between bowel motions to reduce discomfort
Is the process different for children?
Bowel preparation for children follows the same process. However, the medication type, timing, and dosage may differ depending on the clinic you go to and the child’s weight. Typically, a low-fibre or ‘white food’ diet is recommended for 2 days before the procedure, but your child’s specialist will provide specific instructions to follow.
What happens during the colonoscopy?
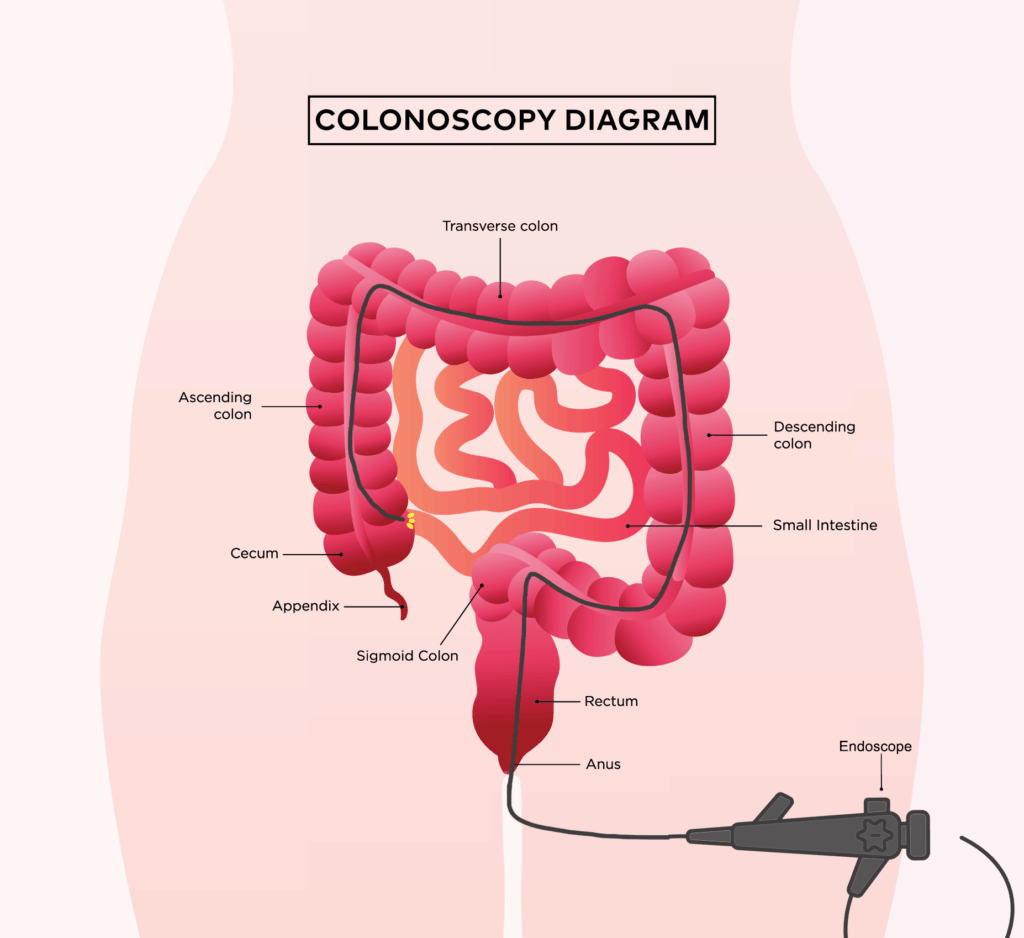
You will lie on your left side on an examination table and receive sedation intravenously (into your veins). Once the sedation takes effect, the specialist will gently inflate the bowel with air and slowly insert the long, flexible tube through the anus, into the rectum and through the colon.
They will closely examine the bowel lining using the camera at the end of the tube, which sends images to a larger screen. You will usually receive images from the procedure afterward if areas of concern are found. The specialist may also take small tissue samples of the colon to be sent for further testing.
Anything that looks suspicious, such as a polyp, can usually be removed during the procedure. If a polyp is too large to remove at the time, they specialist can take a sample of the tissue (known as a biopsy) and send it for testing to determine the nature of the growth. The whole procedure typically takes 20-30 minutes.
What happens after the colonoscopy?
After the procedure, you will be taken to a recovery room and monitored while the sedation wears off. Most people don’t remember the procedure, though some do. You should receive a copy of the report with your results before you go home, and it should also be uploaded to My Health Record. If biopsies were taken, you should get the results within 1 week. If anything of concern is found, your specialist will organise a follow-up plan.
You will need someone to accompany you home, as you can’t drive after the sedation. Plan to rest for the remainder of the day and you should be able to return to normal eating and activities the following day.
You may experience some cramping or bloating due to the air used to inflate the bowel during the procedure. You might see a small amount of blood in your poo or on the toilet paper if you had biopsies taken or polyps removed, but your bowel movements should return to normal within 7 days.
Always follow the specific after-care instructions provided by your specialist and ask for clarification if needed.
What are the risks?
A colonoscopy is generally a very safe procedure with minimal side effects. The most common minor side effects include bloating, nausea, abdominal pain, and vomiting.
More serious risks can occur but are uncommon. These include:
- Bowel tears (perforations): a very rare but serious complication that may require surgery to fix
- Bleeding: more likely if a polyp is removed
- Infection
- Missed polyps or cancer
- Complications from the anaesthesia
Your specialist should help you understand the likelihood of these risks and the benefits of the procedure so that you can make an informed decision before proceeding.
If you experience severe abdominal pain, excessive rectal bleeding, fever, or anything unexpected following the procedure, contact your specialist as soon as possible or go to the emergency department.
How much will I have to pay?
If you have a Medicare card and the procedure is performed in a public hospital, there is no cost to you. However, wait times are extremely variable. Depending on your symptoms, you may wait anywhere from 1 month to as long as 2 years for an appointment through the public system.
If you go through the private health system, you can usually book the procedure within 1-2 weeks, but there will be out-of-pocket costs. Without private health insurance, the cost is typically $1300-$3000 due to fees from the hospital, anaesthetist, and gastroenterologist. The cost depends on the hospital or clinic, and you should get a small Medicare rebate. Your specialist should explain the costs before you book, and you will need to provide informed financial consent before proceeding with the appointment.
If you have private health insurance, most of the cost will be covered, but you may need to pay an excess (usually $500-$750) and a gap fee, depending on the hospital or clinic. If you have already been admitted to the hospital in the same calendar year, the excess is usually waived. Contact your private health fund with the item codes provided by your specialist to confirm what you’ll need to pay.