Blog
New biological pathway and principal driver of IBD discovered
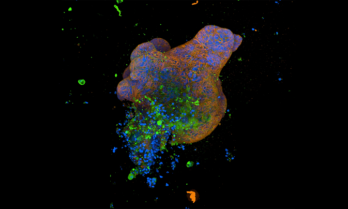
"Researchers at the Francis Crick Institute, working with UCL and Imperial College London, have discovered a new biological pathway that is a principal driver of inflammatory bowel disease (IBD) and related conditions, and which can be targeted using existing drugs."

ABC News report: Rise in IBD diagnoses
An article recently featured in the ABC which discussed the increasing prevalence of Inflammatory Bowel Disease diagnoses in Australia –…
Cambridge University lab grown “mini guts” study
"Cambridge scientists have grown ‘mini-guts’ in the lab to help understand Crohn’s disease, showing that ‘switches’ that modify DNA in gut cells play an important role in the disease and how it presents in patients. These could in future be used to identify the best treatment for an individual patient, allowing for more precise and personalised treatments."

CCA Healthdirect partnership
CCA recently entered into an Information Partnership with Healthdirect Australia. This partnership allows us to share our resources with a wider audience.

10 news & Garvan Institute of Medical Research segment
A segment on 10 News First that aired yesterday on the Garvan Institute of Medical Research autoimmune disease research project.

ABC Radio National interview: supporting kids with IBD and other chronic illnesses in remote locations
Associate Professor Ed Giles and Awareness Month Champion Aiyahna spoke with ABC Host and CCA Ambassador Jacinta Parsons on ABC Radio National's Life Matters program this morning about the care and support received by kids living with IBD and other chronic health diseases across Australia, especially in regional, rural and remote locations.

CCA CEO Joins EFCCA Roundtable discussion in Mexico City
CCA CEO Joins EFCCA Roundtable discussion in Mexico City This year, the central theme for World IBD Day was “IBD…

Crohn’s and Colitis Australia calls for policy changes to save kids’ guts!
Research reveals that young people with IBD aren’t receiving the care they need. Australia, 1 May 2024 – Research has…

Survey on the sexual and reproductive health needs of women in Australia with IBD
Researchers at Western Sydney University and Auckland University of Technology want to understand what the sexual and reproductive health needs are of women who live in Australia with the chronic condition of Inflammatory Bowel Disease.

Inspiring others and raising awareness: Tahlia’s story
I am hoping my story will inspire others and raise awareness for this disease.

“Extending beyond the ordinary” – Aiyahna’s story
We have a magnificent opportunity to teach others around us how to flourish — regardless of their circumstances or the challenges we are facing. So, let’s do this together. Let’s build a team, let’s support each other, let’s lift each other up and let’s make a difference. Let’s make our life stories —despite living with IBD – extend beyond the ordinary. Instead, let's make them extraordinary!

Covid-19 vaccine advice
The Australian Government has accepted the latest advice from the Australian Technical Advisory Group on Immunisation (ATAGI) on the National COVID-19 Vaccine Program for 2024. Adults 65 years and over, or aged 18-64 who are severely immunocompromised, are eligible to receive a booster dose every 6 months.